A recent paper by British and Dutch scientists, currently available on the bioRxiv* preprint server, shows that the neutralizing activity of monoclonal antibodies can be dramatically reduced by mutations of the SARS-CoV-2 spike glycoprotein – unlike polyclonal antibodies generated after natural infection that remain active regardless of any introduced amino acid changes.
Serum neutralization activity is considered the most important correlate of protection against viral infections after natural exposure to the virus or following vaccination. The same is valid for the severe acute respiratory syndrome virus 2 (SARS-CoV-2), a causative agent of the rampant coronavirus disease (COVID-19) pandemic.
Still, efficacious protection is not reliant only on potency but also on an adequate breadth of serum neutralization due to high-level variation in major antigens of certain viruses. The classic example is the influenza virus, where the lack of breadth hampers the generated antibody response's protective capacity.
Therefore, as many novel SARS-CoV-2 are emerging rapidly worldwide (exemplified by the B.1.1.7, P.1, and 501Y.V2 lineages), it is pivotal to understand whether antibody responses induced by the infection with the virus or by currently available vaccines will also be effective against these new variants.
Consequently, a research group led by Dr. Chloe Rees-Spear from the University College London in the United Kingdom decided to appraise the neutralization of a series of mutated spike glycoprotein SARS-CoV-2 pseudotypes – including the infamous B.1.1.7 variant.
Introducing a myriad of point mutations
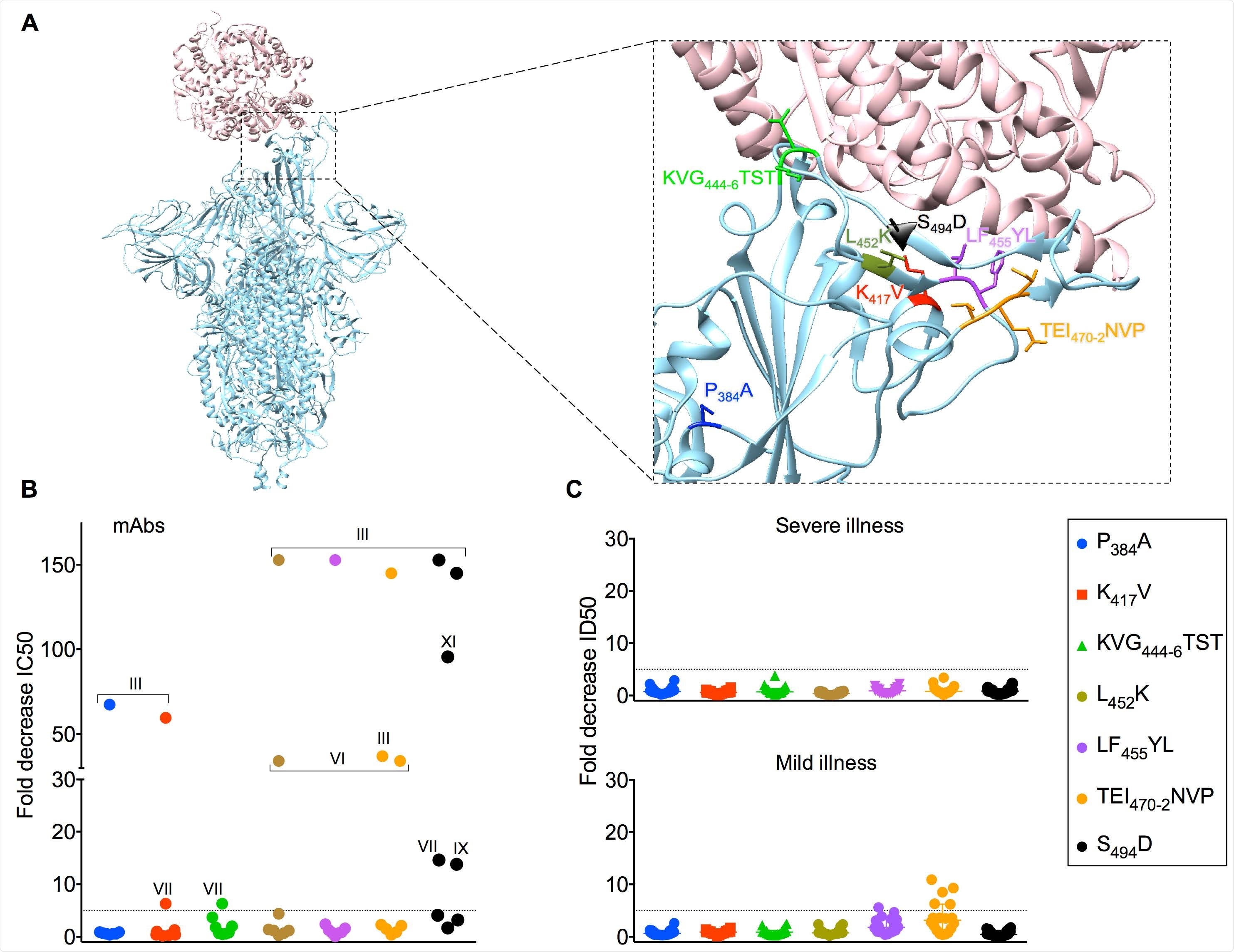
In this study, the researchers evaluated the purported role of individual amino acids in enabling the escape from neutralizing antibodies. Initially, a series of point mutations were made to modify the amino acids in SARS-CoV-2 to match those at analogous position in SARS-CoV (i.e., a causative agent of the original SARS outbreak in 2002/2003).
The next step was to emulate individual point mutations that tend to emerge in the real world by generating a pseudotype virus with the use of the B.1.1.7 variant spike sequence. Viral pseudotype mutants were then screened with highly specific assays.
The end-goal was to assess the impact of SARS-CoV spike glycoprotein substitutions on SARS-CoV-2 monoclonal antibody neutralization, as well as to appraise the impact on serum neutralization. Semi-quantitative enzyme-linked immunosorbent assay (ELISA) was one of the main tools in this endeavor.
Impact on monoclonal antibodies and serum neutralization
In a nutshell, this study has shown that the spike glycoprotein mutations can reduce or eliminate neutralizing activity by individual monoclonal antibodies; on the other hand, serum neutralization was not so strongly affected.
More specifically, only one engineered mutation and none of the perceived spike glycoprotein mutations of the B.1.1.7 variant resulted in an outright escape from neutralizing activity, which was observed for only one out of 36 included serum samples.
"Our results suggest that the majority of vaccine responses should be effective against the B.1.1.7 variant, as the sera evaluated were obtained after infection early in the pandemic when the commonly circulating virus was highly similar in sequence to the vaccines now being deployed", say study authors.
Diminished potency by 5-10 fold was seen in only a small number of samples (i.e., 3 out of 36) interrogated against B.1.1.7 strain; nonetheless, all neutralization titers were still above 1:200 in basically all the cases.
Polyclonal antibody response – a marker of resilience
The most probable explanation of why a greater effect is observed on monoclonal antibodies compared to sera is the intrinsic polyclonality specific for serum neutralization. In other words, when many antibodies target major neutralizing sites in slightly different ways, it is far less sensitive to spike glycoprotein mutations.
"This work highlights that changes in the SARS-CoV-2 spike can alter neutralization sensitivity and underlines the need for effective real-time monitoring of emerging mutations and their impact on vaccine efficacy", explain the authors of this bioRxiv paper.
Likewise, it is also relevant for the potential (and already advocated) use of convalescent plasma, as well as the development of effective therapeutic monoclonal antibodies in our ongoing fight against COVID-19, but also long-term, global management of coronaviruses.
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
https://news.google.com/__i/rss/rd/articles/CBMijAFodHRwczovL3d3dy5uZXdzLW1lZGljYWwubmV0L25ld3MvMjAyMTAxMjEvTmV3LWRhdGEtb24taW1wYWN0LW9mLXNwaWtlLW11dGF0aW9ucy1hbmQtQjExNy1VSy12YXJpYW50LW9uLW5ldXRyYWxpemF0aW9uLWJ5LW1BYnMtYW5kLXNlcmEuYXNweNIBkAFodHRwczovL3d3dy5uZXdzLW1lZGljYWwubmV0L2FtcC9uZXdzLzIwMjEwMTIxL05ldy1kYXRhLW9uLWltcGFjdC1vZi1zcGlrZS1tdXRhdGlvbnMtYW5kLUIxMTctVUstdmFyaWFudC1vbi1uZXV0cmFsaXphdGlvbi1ieS1tQWJzLWFuZC1zZXJhLmFzcHg?oc=5
2021-01-22 03:20:00Z
CAIiEPodyN-AGuhpsffw8WWfgMIqMwgEKioIACIQZdRflS9INK7zM5FkBi3R3CoUCAoiEGXUX5UvSDSu8zORZAYt0dwwr47MBg
Bagikan Berita Ini














0 Response to "New data on impact of spike mutations and B117 UK variant on neutralization by mAbs and sera - News-Medical.Net"
Post a Comment