Using a set of different monoclonal antibodies, researchers determined different mutations in the SARS-CoV-2 spike protein that leads to resistance. Understanding these resistant mutations is important in developing effective therapeutic strategies.
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), responsible for the COVID-19 pandemic, infects host cells via the spike proteins on the virus surface. The N-terminal subunit (S1) plays a role in receptor binding and the C-terminal subunit (S2) helps in the virus-host cell membrane fusion.
The receptor-binding domains (RBDs) of S1 bind to the human angiotensin-converting enzyme 2 (ACE2). SARS-CoV-2 antibodies prevent infection by targeting the RBD.
RNA viruses, like SARS-CoV-2, are present as a swarm of genome sequences around a core sequence. Variants can escape from this swarm in the presence of antibodies or drugs and become resistant.
There are now more than 2,700 mutations identified in the spike protein of the SARS-CoV-2 virus. There may be several mechanisms for these mutations, like host adaptation and immune selection during natural infection. Additional mutants could arise with the use of vaccines, therapeutic antibodies, and convalescent plasma therapy, which may reduce the effectiveness of these therapies.
Mutations that are resistant to antibodies
In a preprint paper published on the bioRxiv* server, researchers from Washington University in St. Louis, Harvard, and Mayo Clinic report on the mutational landscape of resistance in the SARS-CoV-2 RBD using a variety of monoclonal antibodies (mAbs).
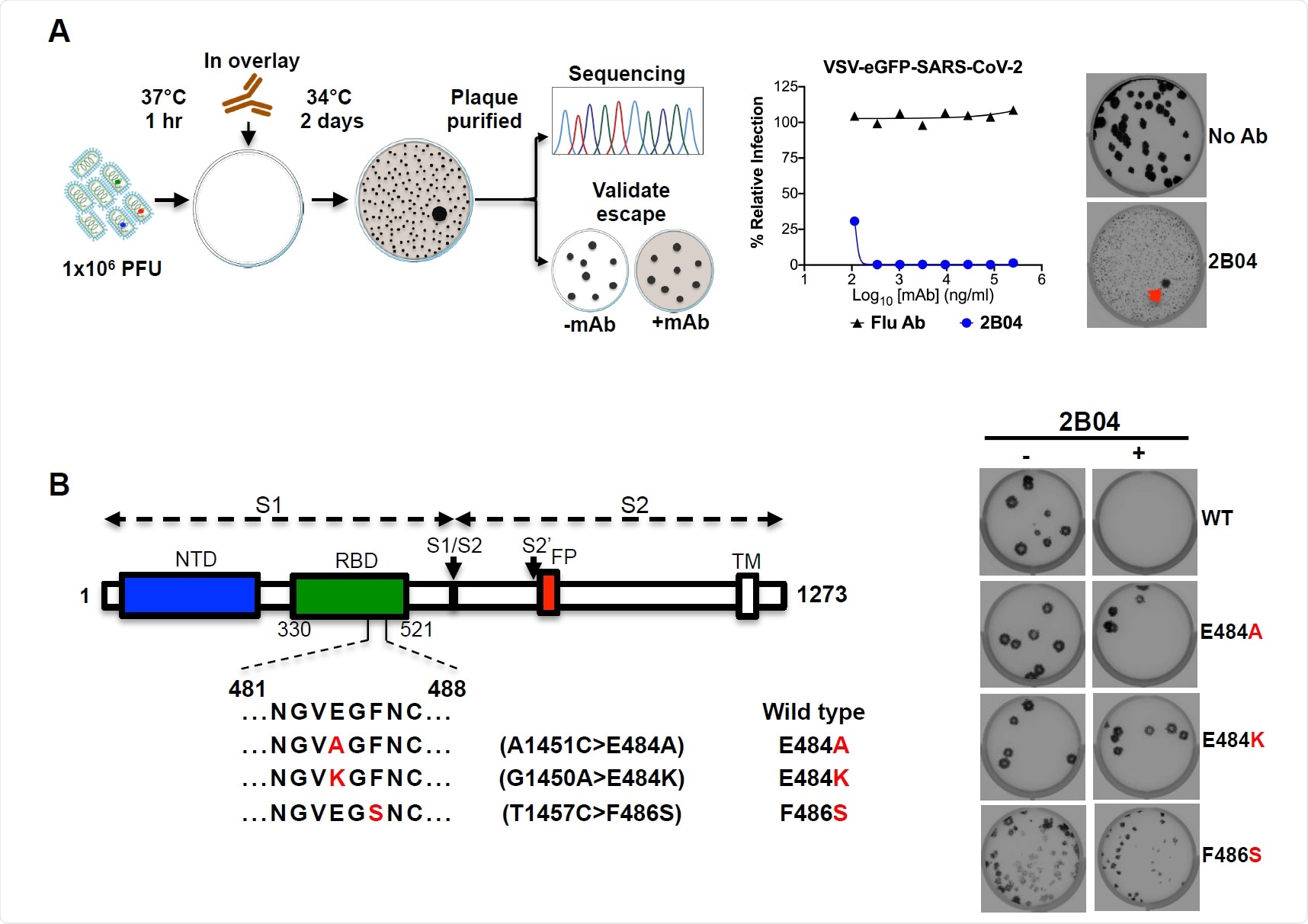
They used a chimeric infectious vesicular stomatitis virus (VSV), a SARS-CoV-2 mimic, where they replaced the glycoprotein with the SARS-CoV-2 spike protein. Using the mAb 2B04, the authors determined that SARS-CoV-2 variants that were not neutralized had mutations in the RBD related to residues involved in ACE2 binding.
Further testing with nine other mAbs revealed a similar result. For the mAb 2H04, the resistance mutations were present outside the ACE2 binding site, on the side and base of the RBD. This suggests virus neutralization may occur by alternative attachment factors.
Several resistance mutations were common among the different mAbs tested, suggesting they represent important antigenic sites on the RBD.
The resistance mutations arising from the different mAbs made them resistant to the other mAbs in the chosen array of mAbs. Substitutions at S477 and E484 led to a broad resistance, while substitutions at several other sites led to resistance to more than one mAb.
Soluble human ACE2 receptors, which are not attached to cells and can compete with those on the host cell to bind to the virus, are another strategy being investigated to combat the virus. The authors tested the resistance of Vero E6 cells to human and murine soluble ACE2. The human soluble ACE2 neutralized all the escape mutants, although some mutations required higher ACE2 concentrations to be neutralized.
The authors also used serum from four convalescent COVID-19 patients to test if the serum antibodies neutralized the escape mutant viruses. They found many mutations that were resistant to neutralization by the sera. In particular, the mutation at residue E484 was resistant to all the four sera, suggesting this is a major neutralizing epitope. However, substitution at this position was quite rare and found only in about 0.05% of strains sequenced.
Resistant mutations found in virus isolates from humans
The authors also tested additional mutations, adding up to 48 different escape mutants. The team also investigated if any of these mutants are present in human isolates of SARS-CoV-2 by compiling available genome sequences of the virus and comparing them against the mutants' genome sequence. They found 27 of the 48 mutations are circulating in humans, with the most frequent mutation seen being D614G, observed in 86% of the isolates.
Substitution at S477N, which conferred a resistance to some level in all the mAbs, was the second most abundant variant in the human isolates.
The authors also note a few limitations of the study. Although the VSV is an effective mimic of the SARS-CoV-2 virus, 27 escape mutants were found only in the human isolates of the virus. They also note the few human sera tested. More human sera samples may help determine the extent of neutralization and escape mutants present.
If such variations in the virus arise after vaccination, they could limit the efficacy of treatment. "The relatively low genetic barrier to resistance combined with knowledge of the presence of relevant substitutions in clinical isolates suggests that effective mAb therapy likely will require a combination of at least two neutralizing antibodies," write the authors. Determining the residues resistant to specific antibodies could help select combinations based on non-overlapping resistant mutations.
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
https://news.google.com/__i/rss/rd/articles/CBMidmh0dHBzOi8vd3d3Lm5ld3MtbWVkaWNhbC5uZXQvbmV3cy8yMDIwMTExMC9JZGVudGlmeWluZy1TQVJTLUNvVi0yLXNwaWtlLXByb3RlaW4tbXV0YXRpb25zLXJlc2lzdGFudC10by1hbnRpYm9kaWVzLmFzcHjSAXpodHRwczovL3d3dy5uZXdzLW1lZGljYWwubmV0L2FtcC9uZXdzLzIwMjAxMTEwL0lkZW50aWZ5aW5nLVNBUlMtQ29WLTItc3Bpa2UtcHJvdGVpbi1tdXRhdGlvbnMtcmVzaXN0YW50LXRvLWFudGlib2RpZXMuYXNweA?oc=5
2020-11-10 08:13:00Z
CAIiENV2Q-kciw-Vp7alBOp5vxYqMwgEKioIACIQZdRflS9INK7zM5FkBi3R3CoUCAoiEGXUX5UvSDSu8zORZAYt0dwww8TIBg
Bagikan Berita Ini














0 Response to "Identifying SARS-CoV-2 spike protein mutations resistant to antibodies - News-Medical.Net"
Post a Comment