As the coronavirus threatens the nation's health care system, hospitals are seeking tens of thousands of ventilators to help patients breathe as the disease attacks their lungs.
But someone needs to operate those breathing machines. And there aren't enough specially trained personnel, health care experts and reports warn.
"They're very complex machines, and you don't have enough respiratory therapists," said Dr. Thomas Frieden, a former director of the U.S. Centers for Disease Control and Prevention.
"You're going to have to train nurses and others to run them," he said. "This is not a surprise. We've known for more than 15 years that this is one of the biggest chokepoints ... in saving lives in a pandemic."
Coronavirus live updates: House set to vote on stimulus; US has most cases on earth; Boris Johnson tests positive
Emergency stockpile: US never spent enough on medical supplies, former managers say
Coronavirus strikes New Orleans: Death rate soars in 'disaster' that could define city for generations
In a race to stave off the collapse of health care systems nationwide, some state regulators are recruiting retired respiratory therapists and trying to speed students in the field to the front lines of the invisible war. Officials in some states may repurpose ventilators used in other parts of hospitals for COVID-19 patients.
The battle against the coronavirus rages hottest in New York City. Sixty percent of the nation's COVID-19 cases are in the metro area, said Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases. Thirteen coronavirus patients died Wednesday in one hospital alone in the borough of Queens and other hospitals were swamped with the ill.
New York is among the states with the lowest concentration of respiratory therapists compared to the national average, according to U.S. Bureau of Labor Statistics data from 2018 that was analyzed by USA TODAY. The concentration is similarly low in Washington, the first hotspot in the U.S.
New York Gov. Andrew Cuomo said Thursday that hospitals in his state are trying to extend the reach of respiratory therapists by pairing two COVID-19 patients on a single ventilator. The strategy, viewed by some health care experts as a potential health risk, has been used in China, Italy, and other countries as patients overwhelmed hospitals.
New York hospitals are also converting anesthesia machines to ventilators, Cuomo said.
Trump questions New York's request for 30,000 more: 'I don’t believe you need 40,000 or 30,000 ventilators'
But even the most drastic of measures might not be enough.
As many as 960,000 COVID-19 patients in U.S. hospital intensive care units could require ventilators to breathe, according to a projection by Dr. James Lawler, an infectious disease specialist at the University of Nebraska Medical Center. The assessment was recently featured in an American Hospital Association webinar.
Shortages of respiratory therapists could limit the number of patients on ventilators to 135,000 at a time, according to a 2015 assessment of the U.S. health care system's capacity during a major health crisis.
It's uncertain whether the entire nation will reach a crisis level at once or whether cases will peak in different areas over time. Virtual lockdowns in some parts of the country are intended to slow transmission of the virus and prevent hospitals from being overwhelmed.
The coronavirus test that wasn't: How federal health officials misled state scientists and derailed the best chance at containment.
Could your December cough actually have been coronavirus? We checked the facts.
Questioning authority in times of crisis is not unpatriotic. It's critical. Read The Backstory from USA TODAY Editor Nicole Carroll.
Bodies could start to stack up from the coronavirus. Coroners and funeral homes say they're ready.
'Who lives and who dies': In worst-case coronavirus scenario, ethics guide choices on who gets care
A scramble to find ventilators and people to operate them
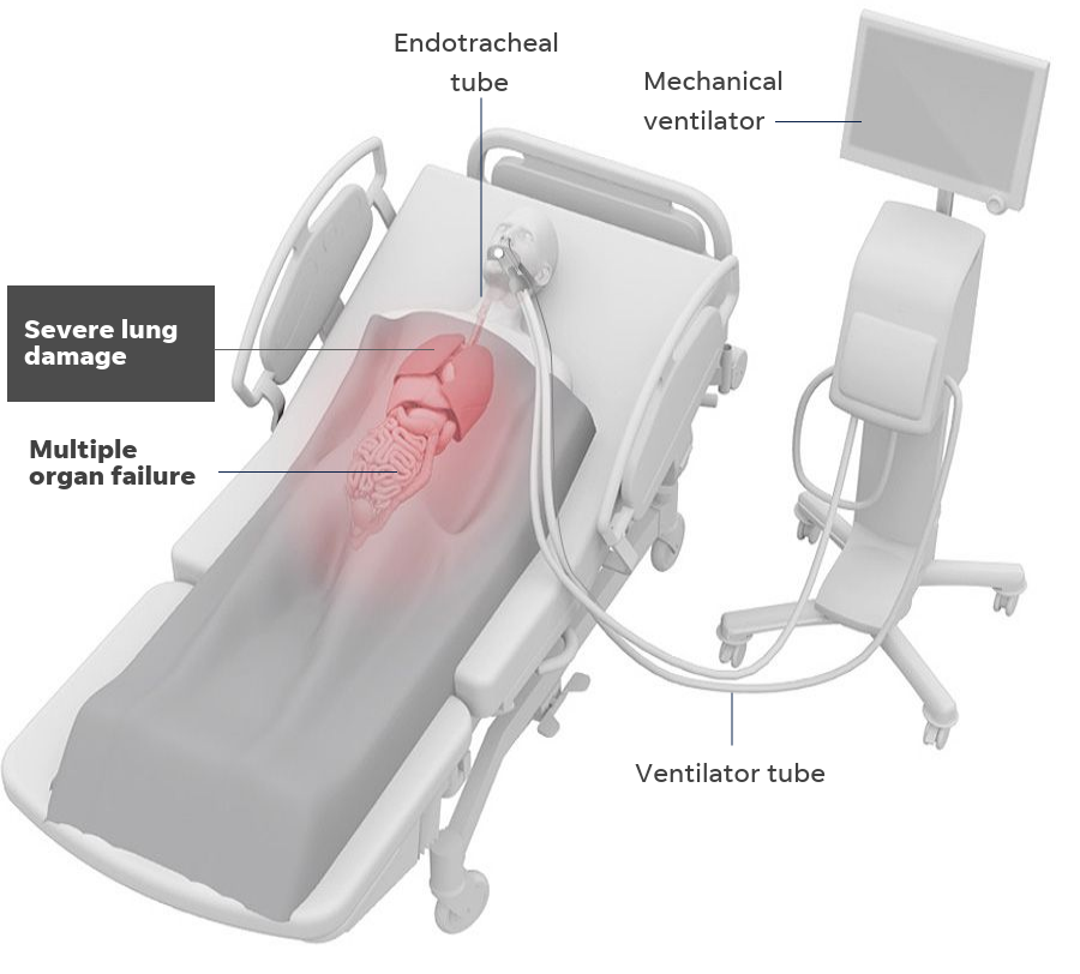
Ventilators are machines that help seriously ill patients breathe by pumping air and oxygen into the lungs through a tube placed in the mouth or nose and reaching into the windpipe. The machine can deliver more oxygen than other methods, and it can also supply pressure to hold the lungs open.
New York alone has asked the Trump administration's coronavirus task force for 30,000 ventilators to supplement the state's supply. The state so far has obtained roughly 11,000, most from the federal government, Cuomo said.
"The number of ventilators we need is so astronomical — it's not like they're in a warehouse," he said Thursday.
COVID-19 patients stay on ventilators for about 11 to 21 days, longer than patients with other respiratory ailments, Cuomo said. That means the machines can't be turned over to others as quickly.
The U.S. has roughly 150,000 respiratory therapists, according to the American Association for Respiratory Care, a nonprofit professional organization. The students must pass board certifications and are licensed by the states where they work.
Their numbers, sufficient for ordinary times, are too few for the pandemic.
And the number of respiratory therapists nationwide is deceptive because it includes those who work for ventilator companies and hold other non-clinical jobs, said Brady Scott, a respiratory therapist who works in Chicago.
“Not all of (the respiratory therapists) are in scrubs with stethoscopes around their necks waiting to take care of patients," Scott said. "We already have other patients who need breathing machines, too. They haven’t all gotten better.”

The respiratory care association decided against trying to train thousands of non-respiratory therapists.
“COVID cases will involve very severe lung damage and damage that is not uniform,” said Timothy Myers, the respiratory care association's chief business officer and a respiratory therapist for 23 years. “It becomes a lot more difficult to take someone not trained and have them monitor the ventilator.”
Instead, the organization is enlisting recent retirees and respiratory therapy students who are approaching graduation.
Roughly 3,000 to 7,000 new respiratory therapists graduate from college each year. The respiratory care association is working with state licensing boards to get temporary or preliminary licenses for students on track to graduate this spring.
As much as 12% of the association's 47,000 members retire each year, according to recent trends. That means there are roughly 10,000 retirees whose licenses have lapsed for less than three years.
Licensing officials in North Carolina, California, Ohio and Colorado told USA TODAY they are cutting red tape to help retirees return quickly.
The respiratory care board of North Carolina, a state with about 5,000 licensed respiratory therapists, approved 50 respiratory therapy students to work as assistants in hospitals. It's working on approvals for dozens more.
The board emailed 900 people with lapsed licenses this week to say they could get relicensed quickly. That generated a huge response, said William Croft, the board's executive director.
“Even prior to this we were struggling to keep up with demand for therapists,” Croft said. One hospital had 20 openings for therapists before the coronavirus crisis.
North Carolina waived continuing education requirements, late renewal fees and many of the requirements to re-apply for a license. The board also made it easier to approve people who are licensed in other states. A process that normally takes weeks now takes two days.

Debra Marlowe answered the call.
The 61-year-old Wilmington, North Carolina, resident was already thinking about coming out of retirement to work part-time as a respiratory therapist before coronavirus started spreading. Then she received Croft's email.
"Seemed like it was meant to be," Marlowe said.
She acknowledged she's concerned about getting sick — older patients are more at risk of getting seriously ill from the virus — but she said that won't stop her from helping where she can.
“I just refuse to worry about it that way,” she said. “We’ve always been exposed to everything.”
In New York, Cuomo cast an even wider net, seeking retirees in many health care specialties. Roughly 40,000 people volunteered to be on call for the state’s newly-created Surge Healthcare Force, including 160 respiratory therapists, according to the governor’s office.
Trying to stay ahead of the curve
A glimpse at conditions in two hospitals, one not yet besieged by the virus and another that's ramping up for the worst, provides a sense of the war.
Scott, the respiratory therapist in Chicago, is a nearly 20-year veteran of the field who splits his time between teaching at Rush University and providing clinical care at Rush University Medical Center.
The hospital was operating normally on Thursday. Its tower, opened in 2012, was the first Chicago-area hospital designed to provide treatment for an infectious disease outbreak.
The Rush emergency department is divided into three 20-bed units. Each unit can be isolated with separate air handling to keep the coronavirus from spreading. And each bed has its own room with a door, not a curtain, unlike many hospitals. That provides additional isolation for each patient.
"But if this were to become the worst type of crisis, nobody has enough equipment and people to deal with it," Scott said.
In New York City, the crisis has transformed the job of Dr. John Puskas — and the hospital where he works.
In ordinary times, the chair of cardiovascular surgery at Mount Sinai - Morningside, a hospital that serves West Harlem and Morningside Heights, near Columbia University, would be performing heart bypasses and more complex procedures.
Two weeks ago, as COVID-19 patients crowded the hospital's intensive care unit, elective surgeries were canceled and cardiovascular surgeons, nurses and other team members were shifted to help treat those felled by the disease.
"We're trying to stay ahead of the curve," Puskas said.
As of mid-day Wednesday, the newly transformed unit was caring for nine coronavirus patients, most on ventilators.
“All of the patients we used to treat were on ventilators, but for different
reasons," Puskas said. “We're quite accustomed to this."
Respiratory therapists “are a resource that’s being increasingly stretched thin,” he said. His team plans to have staffers who are familiar with operating ventilators mentor those who aren't.
"It will be on-the-job emergency training," Puskas said.
As the hospital admits more patients with COVID-19, some ventilators may have to serve two patients at once, he said. They should be paired according to their body and lung size, as well as their airway resistance.
“It will not be optimal,” he said, echoing the view of Scott, the respiratory therapist in Chicago.
Puskas predicted his hospital could handle the load if the surge of COVID-19 patients builds over a few months. However, if the patient load spikes over the next six weeks, “we will run out of ICU units and ventilators and we will not be able to give patients all the level of care they need,” he said.
"We’re not going to quit,” Puskas said. “Everybody here is 100% determined to meet this challenge.”
https://news.google.com/__i/rss/rd/articles/CBMijQFodHRwczovL3d3dy51c2F0b2RheS5jb20vc3RvcnkvbmV3cy9uYXRpb24vMjAyMC8wMy8yNy9jb3JvbmF2aXJ1cy1ob3NwaXRhbHMtZmFjZS1zaG9ydGFnZXMtcmVzcGlyYXRvcnktdGhlcmFwaXN0cy1ydW4tdmVudGlsYXRvcnMvMjkxNDYzNTAwMS_SASdodHRwczovL2FtcC51c2F0b2RheS5jb20vYW1wLzI5MTQ2MzUwMDE?oc=5
2020-03-27 15:53:33Z
52780692791893
Bagikan Berita Ini














0 Response to "'On-the-job emergency training': Hospitals may run low on staff to run ventilators for coronavirus patients - USA TODAY"
Post a Comment